By Martha Funnell, MS, RN, CDE Have you ever wondered how your doctor knows what to do, or why treatments change over time? Most healthcare providers today use “Standards of Care” to guide their decisions. In diabetes, the standards from the American Diabetes Association (ADA) are commonly used. Each year, the ADA reviews findings from all of the diabetes studies and revises its guidelines based on the results. The 2013 guidelines were recently published. One of the changes in this year’s guidelines is in the blood pressure target. 1?BLOOD PRESSURE FACTS Blood pressure is the amount of pressure on your blood vessel walls when your heart is pumping (top number) and between?beats (bottom?number). Along with high blood glucose levels, high blood pressure increases your risk for strokes, heart attacks, kidney damage and eye disease. If you have been told you have high blood pressure (hypertension), it means the top (systolic) number is too high, the bottom (diastolic) number is too high or both are too high. 2?NEW TARGETS FOR BLOOD PRESSURE The new target blood pressure guideline for people with diabetes is less than 140/80?mmHg. The previous?target was less than?130/80 mmHg. This?change was made because studies have shown that there is no benefit to lowering the blood pressure from 140/80 to 130/80 mmHg. The risk for a heart attack, stroke, kidney damage and death is about the same at less than 140/80 or 130/80 mmHg. 3?KEYS TO SUCCESS Although this may seem like a change from the past target of 130/80 mmHg, it is only part of the picture. Normal blood pressure for everyone, including people with diabetes, is still 120/80 mmHg. If your blood pressure is between 120/80 and 140/80 mmHg, lifestyle changes, such as weight loss, physical activity or a DASH eating plan, are recommended. If your blood pressure is 140/80 mmHg or higher, your healthcare provider is likely to prescribe medicine to help you reach your target. If your blood pressure is less than 140/80 mmHg, if you have no other health problems and can reach the less than 130/80 mmHg target without any “undue burden” (such as cost or side effects from blood pressure medicines), your target may still be lower than 130/80 mmHg. Talk with your provider about your blood pressure and the best target for you. HELP REACH YOUR TARGET BLOOD PRESSURE YOU CAN: lose weight and keep it off take your blood pressure medicine regularly change the dose or type of blood pressure medicine eat more vegetables, fruits, whole grains and low-fat dairy products stop smoking eat less salt and salty foods exercise more
The post Reach Your Target Blood Pressure appeared first on Spring 2017 Issue | CDiabetes Online Magazine.
]]>
The post Reach Your Target Blood Pressure appeared first on Spring 2017 Issue | CDiabetes Online Magazine.
]]>
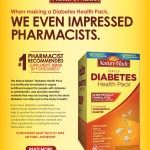
The post No Charge OneTouch? Meter Coupon appeared first on Spring 2017 Issue | CDiabetes Online Magazine.
]]>
The post No Charge OneTouch? Meter Coupon appeared first on Spring 2017 Issue | CDiabetes Online Magazine.
]]>
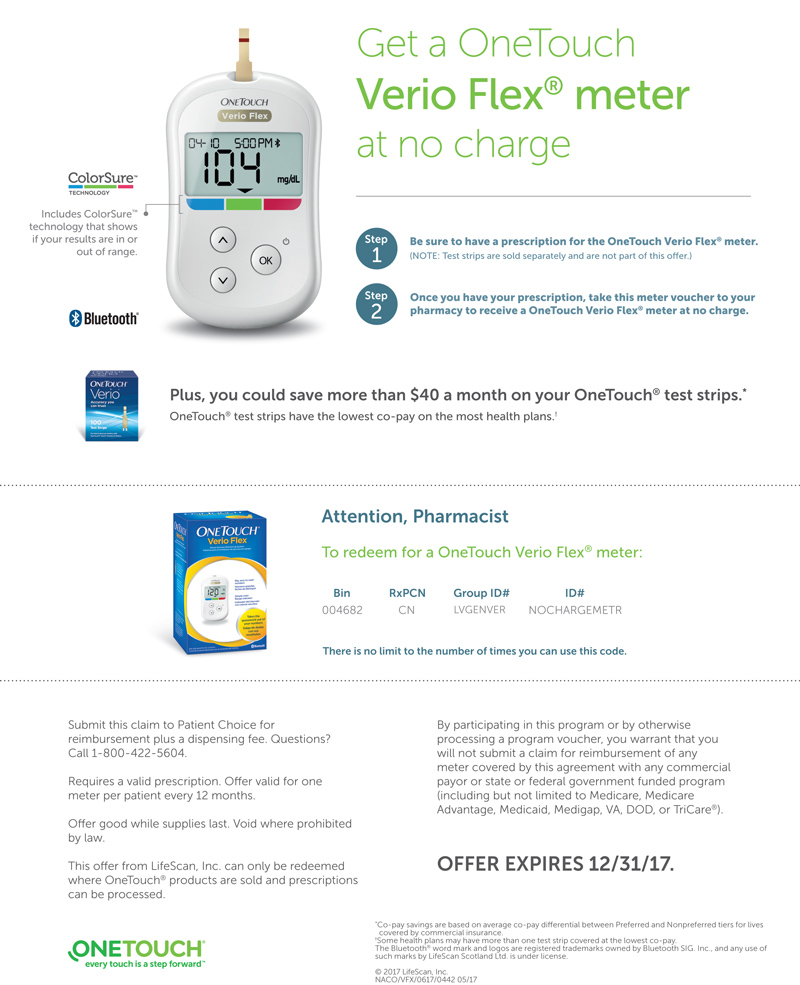
In order to live an active and mobile lifestyle, it is important to positively promote your joint health. So, what is joint health? The joint is where our bones connect and it is a complex structure of many specialized tissues that function together to provide the means for motion. Inside the joint, there is cartilage and viscous fluid. The cartilage is resilient with tremendous shock absorbing capability while the viscous fluid bathes and lubricates the joint. As a consequence of aging, trauma, and wear and tear on the joint, cartilage may be broken down, which can compromise joint movement. In order to remain active and live a healthy lifestyle, it is critically important to take care of your joints. How can I promote joint health? There are many ways to promote your joint health such as: eating healthy staying active and maintaining a healthy weight visiting your healthcare provider regularly taking your medications as prescribed taking dietary supplements You should also consider taking a high quality glucosamine and chondroitin sulfate supplement. Glucosamine, in combination with chondroitin sulfate, helps inhibit enzymes responsible for the breakdown of cartilage and supports the maintenance of healthy joints. Choosing the right glucosamine/chondroitin product Recent published clinical studies have further validated the combination of high quality glucosamine/chondroitin supplementation for joint health. It is important to make sure you purchase a high quality glucosamine/chondroitin combination product, and below are some of the items to look for: Reputable brand cited in published clinical studies Serving size of trademarked active ingredients are the same as used in clinical studies Quality seal from third party public health and safety organizations Take away message It is important to closely monitor and take care of your joints to remain active late in life. It is recommended to consult your physician before taking any medication or dietary supplement.
The post Introduction to Joint Health appeared first on Spring 2017 Issue | CDiabetes Online Magazine.
]]>
In order to live an active and mobile lifestyle, it is important to positively promote your joint health. So, what is joint health? The joint is where our bones connect and it is a complex structure of many specialized tissues that function together to provide the means for motion. Inside the joint, there is cartilage and viscous fluid. The cartilage is resilient with tremendous shock absorbing capability while the viscous fluid bathes and lubricates the joint. As a consequence of aging, trauma, and wear and tear on the joint, cartilage may be broken down, which can compromise joint movement. In order to remain active and live a healthy lifestyle, it is critically important to take care of your joints.
How can I promote joint health?
There are many ways to promote your joint health such as:
- eating healthy
- staying active and maintaining a healthy weight
- visiting your healthcare provider regularly
- taking your medications as prescribed
- taking dietary supplements
You should also consider taking a high quality glucosamine and chondroitin sulfate supplement. Glucosamine, in combination with chondroitin sulfate, helps inhibit enzymes responsible for the breakdown of cartilage and supports the maintenance of healthy joints.
Choosing the right glucosamine/chondroitin product
Recent published clinical studies have further validated the combination of high quality glucosamine/chondroitin supplementation for joint health. It is important to make sure you purchase a high quality glucosamine/chondroitin combination product, and below are some of the items to look for:
- Reputable brand cited in published clinical studies
- Serving size of trademarked active ingredients are the same as used in clinical studies
- Quality seal from third party public health and safety organizations
Take away message
It is important to closely monitor and take care of your joints to remain active late in life. It is recommended to consult your physician before taking any medication or dietary supplement.
The post Introduction to Joint Health appeared first on Spring 2017 Issue | CDiabetes Online Magazine.
]]>
The post Cosamin ? ASU for Joint Health appeared first on Spring 2017 Issue | CDiabetes Online Magazine.
]]>
The post Cosamin ? ASU for Joint Health appeared first on Spring 2017 Issue | CDiabetes Online Magazine.
]]>
By Erin Palinski-Wade RD, LDN, CDE When it comes to controlling your blood glucose, you have probably researched the impact of everything from food, to exercise, to weight control. But have you looked into how spices may impact it? Cinnamon is a spice that doesn’t just add great flavor to foods; it may help to lower blood glucose as well. The best benefit it offers is that it’s all-natural and considered safe for most people with diabetes. Does it sound too good to be true? In Medieval times, cinnamon was used for medicinal purposes thanks to its high antioxidant properties. Research now shows us that it may be a powerful player in the fight against diabetes. Cinnamon may help to lower blood glucose levels by decreasing insulin resistance. When your cells become resistant to insulin, the glucose-lowering hormone in your body, they do not allow insulin to carry glucose into your cells. This results in glucose remaining in your bloodstream and rising over time, eventually leading to diabetes. Both whole cinnamon and extracted cinnamon have been shown to lower blood glucose levels. Cinnamon has also been shown to help reduce unhealthy LDL cholesterol levels and blood pressure, both of which are conditions that can increase your risk of heart disease. One down side is that everything that Mother Nature puts into the cinnamon plant also ends up in the finished product. This includes water soluble as well as fat soluble compounds. Our bodies have no problem processing water soluble compounds, but fat soluble compounds tend to be stubborn for our bodies to digest. When choosing a form of cinnamon, we suggest you look for a water extracted concentrate without the fat soluble compounds. Water extracted forms can maximize the health benefits, while minimizing the risks of fat soluble buildup. The extraction process allows the beneficial water soluble components of cinnamon to stay, providing you with the same health benefits of whole cinnamon in a much smaller portion. When looking for water extracted cinnamon, it’s important that you read the label and look specifically for the term “water extracted.” Because it is more concentrated, you can take fewer capsules to get all the health benefits of cinnamon. This may be more practical than trying to incorporate large amounts of whole cinnamon into your meal plan. CinSulin Water-extracted cinnamon is backed by five human clinical studies, all of which are double blind, peer reviewed and published. In addition, UC Davis completed a meta analysis to validate the results of these human clinical studies. They found support that water extracted cinnamon lowered fasting blood glucose an average of 10%. If you are considering using cinnamon to help control blood glucose levels, make sure you discuss this with your certified diabetes educator or other healthcare provider. If you use cinnamon in combination with other medicines or supplements that also lower glucose levels, you may increase your risk of hypoglycemia. Your healthcare provider can work with you to make sure you incorporate cinnamon into your diabetes treatment plan in a way that works best for you.
The post How Water Extracted Cinnamon Can Improve Your Blood Glucose Control appeared first on Spring 2017 Issue | CDiabetes Online Magazine.
]]>
By Erin Palinski-Wade RD, LDN, CDE
When it comes to controlling your blood glucose, you have probably researched the impact of everything from food, to exercise, to weight control. But have you looked into how spices may impact it? Cinnamon is a spice that doesn’t just add great flavor to foods; it may help to lower blood glucose as well. The best benefit it offers is that it’s all-natural and considered safe for most people with diabetes.
Does it sound too good to be true? In Medieval times, cinnamon was used for medicinal purposes thanks to its high antioxidant properties. Research now shows us that it may be a powerful player in the fight against diabetes.
Cinnamon may help to lower blood glucose levels by decreasing insulin resistance. When your cells become resistant to insulin, the glucose-lowering hormone in your body, they do not allow insulin to carry glucose into your cells. This results in glucose remaining in your bloodstream and rising over time, eventually leading to diabetes. Both whole cinnamon and extracted cinnamon have been shown to lower blood glucose levels. Cinnamon has also been shown to help reduce unhealthy LDL cholesterol levels and blood pressure, both of which are conditions that can increase your risk of heart disease.
One down side is that everything that Mother Nature puts into the cinnamon plant also ends up in the finished product. This includes water soluble as well as fat soluble compounds. Our bodies have no problem processing water soluble compounds, but fat soluble compounds tend to be stubborn for our bodies to digest.
When choosing a form of cinnamon, we suggest you look for a water extracted concentrate without the fat soluble compounds. Water extracted forms can maximize the health benefits, while minimizing the risks of fat soluble buildup. The extraction process allows the beneficial water soluble components of cinnamon to stay, providing you with the same health benefits of whole cinnamon in a much smaller portion.
When looking for water extracted cinnamon, it’s important that you read the label and look specifically for the term “water extracted.” Because it is more concentrated, you can take fewer capsules to get all the health benefits of cinnamon. This may be more practical than trying to incorporate large amounts of whole cinnamon into your meal plan.
CinSulin Water-extracted cinnamon is backed by five human clinical studies, all of which are double blind, peer reviewed and published. In addition, UC Davis completed a meta analysis to validate the results of these human clinical studies. They found support that water extracted cinnamon lowered fasting blood glucose an average of 10%.
If you are considering using cinnamon to help control blood glucose levels, make sure you discuss this with your certified diabetes educator or other healthcare provider. If you use cinnamon in combination with other medicines or supplements that also lower glucose levels, you may increase your risk of hypoglycemia. Your healthcare provider can work with you to make sure you incorporate cinnamon into your diabetes treatment plan in a way that works best for you.
The post How Water Extracted Cinnamon Can Improve Your Blood Glucose Control appeared first on Spring 2017 Issue | CDiabetes Online Magazine.
]]>
The post trunature? Advanced Strength CinSulin?, 170 Capsules appeared first on Spring 2017 Issue | CDiabetes Online Magazine.
]]>
The post trunature? Advanced Strength CinSulin?, 170 Capsules appeared first on Spring 2017 Issue | CDiabetes Online Magazine.
]]>
By Martha Funnell, MS, RN, CDE YOUR BODY AND WEIGHT LOSS When you start to lose weight, you lose some of your stored fat. That may seem like a good thing to you, but your body doesn’t always agree. We used to think fat just sat in your body and did nothing. But we now know that is not true. The fat you store makes hormones that help control your weight and hunger. THE ROLE OF LEPTIN Leptin is a hormone made in the fat cells that goes through your bloodstream to your brain. Leptin tells your brain when you are full so that you stop eating. The more overweight you are, the more leptin your body makes. Over time, your body becomes resistant to these very high levels of leptin. The leptin is blocked from giving your brain the message that you are full. In addition, food is more rewarding when you are resistant to leptin. You eat more, enjoy it less and feel hungry. As you lose weight, your leptin levels begin to drop. Because of this, your body thinks you are starving. Your metabolism slows down and tries to hang on to the fat you have stored. Other signals also tell your brain you are hungry, so you want to eat more, as well. In some ways, you fight with your body when you try to lose weight. Unfortunately, you can’t take leptin to lose weight. Leptin is a protein and would be broken down in the stomach before it could get into the bloodstream. YOUR SET-POINT WEIGHT The other thing to keep in mind is that some experts believe everyone has a built-in control system that decides how much he or she should weigh. This set point is different for everyone and is set by your genes. That’s why it is easier to lose weight when you begin dieting than later on in your weight-loss efforts. You may do the same things, but you stay at the same weight or even regain what you lost. Your metabolism slows down because your body is trying to get back to your set-point weight. The set-point also affects how many calories it takes to maintain your weight. If you lost weight and now weigh 150 pounds, you will need fewer calories to maintain that weight than a person who has always weighed 150 pounds. And now for the good news: Although it may sound impossible, you can lose weight and keep it off. Exercise helps lower insulin resistance, which can decrease leptin levels. Exercise can also help increase your metabolism and fight your body’s resistance to weight loss. It isn’t easy and it isn’t as simple as others tell you, but it can be done. Take it one meal and one day at time and you can do it. Although it may sound impossible, you can lose weight and keep it off. Although it may sound impossible, you can lose weight and keep it off.
The post The Skinny On Weight Loss appeared first on Spring 2017 Issue | CDiabetes Online Magazine.
]]>
The post The Skinny On Weight Loss appeared first on Spring 2017 Issue | CDiabetes Online Magazine.
]]>
By Martha Funnell, MS, RN, CDE Along with anger, fear and frustration, guilt is a common feeling among people with diabetes. No matter how much you do to care for yourself, it seems as if there is always more you could have done. After all, if you walked for 10 minutes, maybe you could have walked for 20. If you skipped dessert at dinner, maybe you should have skipped the bread, as well. If you feel guilty, it can add to the stress you feel living with diabetes. It can also cause you to have very negative feelings about diabetes in general. Here are some ideas to help get off the guilt trip and feel better about your efforts and yourself. ? TAKE TIME TO FEEL GOOD ABOUT WHAT YOU DID. Don’t focus on what you did wrong. Instead, take time every day to think about what you did right. After all, no one is perfect. It’s what you do most of the time that matters. At the end of every day, mentally list or write down on paper all you did to care for your diabetes. Focus on the positives to help inspire you to keep working on your diabetes. ? THERE IS NO SUCH THING AS FAILURE. Don’t think about whether you were a success or a failure, think of what you learned. Ask yourself what you tried and how it worked. If it worked, ask yourself why. If it did not work, ask yourself what got in the way and what you might do differently tomorrow. ? USE YOUR GUILT. Don’t feel bad: turn your negative feelings into positive energy. It may sound odd, but some people use guilt as an excuse for the choices they make. It’s as if they say, “Well, I didn’t do what I wanted to do, but I feel bad about it so it’s OK.” Feeling guilty does not change your results. And if it doesn’t change what you do the next time, then it is not helping you. Don’t use guilt as an excuse: use it to motivate yourself as you make choices throughout the day. ? FOCUS ON TOMORROW. Guilt is about what you did in the past. No matter how much guilt you feel, you cannot change what already happened. Don’t waste your time feeling guilty on what you can no longer change. Focus instead on what you can do tomorrow. ? CHOOSE ONE THING YOU KNOW YOU CAN DO. Don’t try to do it all and then feel bad when you can’t get everything done. Pick one thing to work on each day. A good place to start is with your biggest struggle or the thing that causes you the most guilt. Take another step toward your goal every few days. ? FEEL GOOD ABOUT YOURSELF. Diabetes care is hard work. Find someone (or several people) who can give you support and cheer you on. Take time to reward yourself for all of the effort you make. Pat yourself on the back for all you do. You’ve earned it. If you feel guilty, it can add to the stress you feel living with diabetes.
The post Pat Yourself On The Back appeared first on Spring 2017 Issue | CDiabetes Online Magazine.
]]>
The post Pat Yourself On The Back appeared first on Spring 2017 Issue | CDiabetes Online Magazine.
]]>
By Johanna Burani, MS, RD, CDE We all live very busy lives, so it can be hard to find time for exercise. We use cars, machines and tools to help us get our work done faster. But those things take away much of our daily movement. So we must plan to keep our bodies moving. Why? Because moving the body is good for it. EXERCISE AND DIABETES If you have type 1 diabetes, ask your doctor or diabetes educator how to lower the amount of insulin you take when you exercise. You don’t want your blood glucose to drop too low. Always check your blood glucose level before and after exercise. If you work out for a long time, you may need to check during your activity. Never exercise on an empty stomach: Eat a snack before or right after your exercise and drink water while you are exercising. It is also a good habit to carry glucose tablets or gel or some other fast-acting sugar source with you in case you feel weak during your exercise. If you have type 2 diabetes and take insulin, follow the same rules as for type 1. If you take oral medicines or no drugs at all for your diabetes, it is still good to speak to your doctor or diabetes educator about your exercise plans. Test your blood glucose level before and after exercise to see if you need a snack. That will also show you to what extent exercise affects your blood glucose level. If you exercise for a long time, be sure to bring along a snack, such as fruit or yogurt. And always have water with you to drink. EXERCISE GUIDELINES The American Diabetes Association recommends people with prediabetes and diabetes to be physically active at least 150 minutes every week. That means 30 minutes of exercise five days a week. To do so, you can walk, play softball, mow the lawn, clean the house, take an exercise class or anything else you like to do. You can wear a pedometer on your belt or waistband. That small tool counts how many steps you take each day. A good long-term goal is to reach 10,000 steps every day. It is common sense to start at a comfortable level and increase the time and speed of your exercise over a period of time. To get the most from your exercise, do it most days every week throughout the year. 5 tips for feeling your best during and after exercise: ? Plan your exercise Plan your exercise. Think about what you can and want to do. Choose what days, what time, for how long and what you will do. Try to follow your plan. ? Eat the right meals Eat a meal that contains carbohydrates one–three hours before you exercise. Examples: a sandwich or breakfast cereal, milk and fruit. ? Drink water Drink 8 ounces of water 20 minutes before starting your exercise. Do not drink ice cold water, which may give you stomach cramps. Drink 8 ounces of water every 20–30 minutes during your exercise. ? Check your blood glucose Check your blood glucose level before and after you exercise. Also check during a long exercise or if you don’t feel right. And you may need to check your blood glucose level during the night if you have exercised for a long time or did intense or unusual activities. That’s to make sure your blood glucose level doesn’t drop too low while you are asleep. ? Speak to your doctor Always talk with your doctor or diabetes educator before you start an exercise program. Make sure they agree on your exercise plan.
The post Exercise: It’s Good For Your Diabetes appeared first on Spring 2017 Issue | CDiabetes Online Magazine.
]]>
The post Exercise: It’s Good For Your Diabetes appeared first on Spring 2017 Issue | CDiabetes Online Magazine.
]]>
The post Find The Test Strip Brand With The Lowest Co-Pay appeared first on Spring 2017 Issue | CDiabetes Online Magazine.
]]>
The post Find The Test Strip Brand With The Lowest Co-Pay appeared first on Spring 2017 Issue | CDiabetes Online Magazine.
]]>
By Robert Ehrman, MD If you have diabetes, you probably know that you are at an increased risk for problems with your eyes, feet, skin?and nervous system. Did you know that diabetes can also cause problems in your mouth? Take Care Of Your Teeth Poor blood glucose control lets bacteria grow easily in your mouth. Having lots of bacteria in your mouth lead to?plaque buildup on your teeth. When this happens, your gums begin to pull away from your teeth, and pockets form between your teeth and gums. These pockets can become filled with germs and small bits of food. The gums then become inflamed and may bleed when you eat or brush your teeth. This condition is called “gingivitis”. Keeping your gums healthy is important because they help to hold your teeth in place. If nothing is done, you can get an infection in your gums that can go on to destroy the bone around your teeth, and they may start to move. Your teeth may fall out or need to be pulled. A recent study at the University of Copenhagen in Denmark looked at the link between oral health and diabetes. The study found that people with good oral health practices, along with a healthy diet and good stress management, had?lower blood glucose levels and healthier teeth and gums. Diabetes: A Major Cause Of Gum Disease There are many causes of gum disease, including smoking, hormonal changes, and certain cancers. Some medicines can?make your mouth dry, which can increase your risk for tooth and gum problems. This is because saliva helps slow the growth of bacteria and keeps your mouth healthy overall. Poorly controlled diabetes can also lead to gum disease. High levels of sugar in saliva make it easy for bacteria to grow there. This is why poorly controlled diabetes is a risk factor for gum disease. Also, diabetes can cause problems with blood flow to your teeth and gums. This makes it harder to repair damage to your gums and fight infection. It is also important to understand that if you develop gum disease from poor oral habits or other reasons, this could make it harder for you to control your diabetes. Other oral problems related to diabetes include: Thrush: this is an infection caused by a fungus that grows in the mouth and throat Dry mouth: this can cause soreness, ulcers, infections and cavities Dental Check-ups Are Important It’s important that you tell your dentist if you have diabetes, and keep them informed of any changes in your condition or medicines. Postpone any non-emergency dental procedures if your blood sugar is not well controlled. What Can You Do To Keep Your Mouth Healthy? The most important thing you can do is control your blood glucose levels. Have dental check-ups every six months?if possible. Avoid smoking and, if you wear dentures, remove and clean them every day. Good blood glucose control can also help prevent or relieve the dry mouth diabetes can cause. Here are some simple tips for a healthy mouth: Keep your blood glucose level under control Brush and floss every day Visit your dentist at least every 6 months. Be sure to tell them that you have diabetes Tell your dentist if your dentures do not fit right, or if your gums are sore Stop smoking. Your healthcare provider or dentist can tell you about what options there are to help you quit Call your dentist if you notice a problem. Take time to check your mouth regularly for any problems. If your gums bleed when you brush or floss, or if you notice dryness, soreness, white patches, or a bad taste in your mouth, contact your dentist right away. Remember, good blood glucose control can help keep your mouth happy and healthy for years to come. 6 Signs Of Gum Disease Red or swollen gums Gums that bleed easily when brushing or flossing Receding gums (pulling away from teeth) Loose teeth, making it hard to bite and chew Constant bad breath Dentures that don’t fit anymore
The post Oral Health And Diabetes appeared first on Spring 2017 Issue | CDiabetes Online Magazine.
]]>
By Robert Ehrman, MD
If you have diabetes, you probably know that you are at an increased risk for problems with your eyes, feet, skin?and nervous system. Did you know that diabetes can also cause problems in your mouth?
Take Care Of Your Teeth
Poor blood glucose control lets bacteria grow easily in your mouth. Having lots of bacteria in your mouth lead to?plaque buildup on your teeth. When this happens, your gums begin to pull away from your teeth, and pockets form between your teeth and gums. These pockets can become filled with germs and small bits of food. The gums then become inflamed and may bleed when you eat or brush your teeth. This condition is called “gingivitis”.
Keeping your gums healthy is important because they help to hold your teeth in place. If nothing is done, you can get an infection in your gums that can go on to destroy the bone around your teeth, and they may start to move. Your teeth may fall out or need to be pulled.
A recent study at the University of Copenhagen in Denmark looked at the link between oral health and diabetes. The study found that people with good oral health practices, along with a healthy diet and good stress management, had?lower blood glucose levels and healthier teeth and gums.
Diabetes: A Major Cause Of Gum Disease
There are many causes of gum disease, including smoking, hormonal changes, and certain cancers. Some medicines can?make your mouth dry, which can increase your risk for tooth and gum problems. This is because saliva helps slow the growth of bacteria and keeps your mouth healthy overall. Poorly controlled diabetes can also lead to gum disease.
High levels of sugar in saliva make it easy for bacteria to grow there. This is why poorly controlled diabetes is a risk factor for gum disease. Also, diabetes can cause problems with blood flow to your teeth and gums. This makes it harder to repair damage to your gums and fight infection. It is also important to understand that if you develop gum disease from poor oral habits or other reasons, this could make it harder for you to control your diabetes.
Other oral problems related to diabetes include:
- Thrush: this is an infection caused by a fungus that grows in the mouth and throat
- Dry mouth: this can cause soreness, ulcers, infections and cavities
Dental Check-ups Are Important
It’s important that you tell your dentist if you have diabetes, and keep them informed of any changes in your condition or medicines. Postpone any non-emergency dental procedures if your blood sugar is not well controlled.
What Can You Do To Keep Your Mouth Healthy?
The most important thing you can do is control your blood glucose levels. Have dental check-ups every six months?if possible. Avoid smoking and, if you wear dentures, remove and clean them every day. Good blood glucose control can also help prevent or relieve the dry mouth diabetes can cause.
Here are some simple tips for a healthy mouth:
- Keep your blood glucose level under control
- Brush and floss every day
- Visit your dentist at least every 6 months. Be sure to tell them that you have diabetes
- Tell your dentist if your dentures do not fit right, or if your gums are sore
- Stop smoking. Your healthcare provider or dentist can tell you about what options there are to help you quit
- Call your dentist if you notice a problem.
Take time to check your mouth regularly for any problems. If your gums bleed when you brush or floss, or if you notice dryness, soreness, white patches, or a bad taste in your mouth, contact your dentist right away. Remember, good blood glucose control can help keep your mouth happy and healthy for years to come.
6 Signs Of Gum Disease
- Red or swollen gums
- Gums that bleed easily when brushing or flossing
- Receding gums (pulling away from teeth)
- Loose teeth, making it hard to bite and chew
- Constant bad breath
- Dentures that don’t fit anymore
The post Oral Health And Diabetes appeared first on Spring 2017 Issue | CDiabetes Online Magazine.
]]>
The post Colgate Total? Toothpaste appeared first on Spring 2017 Issue | CDiabetes Online Magazine.
]]>
The post Colgate Total? Toothpaste appeared first on Spring 2017 Issue | CDiabetes Online Magazine.
]]>
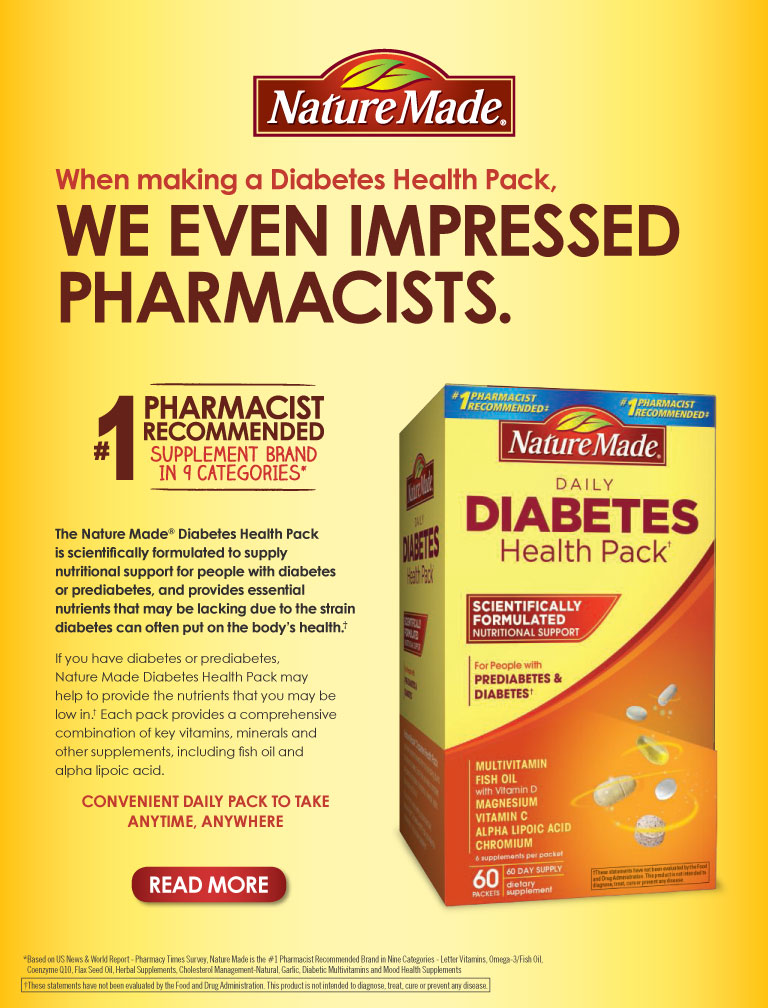
The post Nature Made? Diabetes Health Pack, 60 Packets appeared first on Spring 2017 Issue | CDiabetes Online Magazine.
]]>
The post Nature Made? Diabetes Health Pack, 60 Packets appeared first on Spring 2017 Issue | CDiabetes Online Magazine.
]]>
By Robert Ehrman, MD ? Reviewed by Fran Daniel, MPH First, it is important to note that eating a variety of whole foods is a better choice for staying healthy than relying on vitamins or supplements.?Eating lean meats, vegetables, fruits, and whole grains- and limiting fats and sugar — are important for keeping your blood glucose under control. Individual foods can give you many different vitamins, minerals, and nutrients, in one?serving. For example, raspberries contain vitamin C, fiber, and antioxidants. These nutrients, plus all?the food nutrients we have not yet discovered, work?together in your body to ensure that you benefit from all of them. Using vitamins or supplements – which do not have the full range of nutrients that whole foods do — may not?be needed unless you have a specific vitamin deficiency. (“Deficiency” means that your body does not have enough?of an important nutrient.) It’s a good idea to talk to your healthcare provider before taking any vitamin supplements to see if you really need them. Your healthcare provider may want you to take?vitamin supplements if you are: On a low-calorie diet and do?not eat a wide variety of foods On a vegan diet (no meat, fish, eggs or dairy products) Pregnant On a restricted diet because you?have food allergies, kidney disease?or have trouble absorbing nutrients What Vitamins Are The Best? Many people, including those with diabetes, may?need to take vitamin D supplements.?Experts say to take 400 international units (IU) each day. Recent studies suggest that this may not be enough vitamin D. Ask your healthcare provider if you ?should take vitamin D supplements,?and how much to take every day. Why Is Vitamin D So Important For Good Health? Vitamin D might be able to: improve pain and tingling in your legs, feet, hands, and fingers. keep bones healthy and strong help with blood glucose control help ease depression in women with type 2 diabetes. How Can I Get More Vitamin D? Go outside in the sunshine. Sunshine is a great way to get vitamin D. To be safe, first check with your healthcare provider to make sure it’s safe for you to spend time in the sun. Eat more fish and egg yolks. Eat cereals with vitamin D added. Drink milk with vitamin D added. Take Vitamin D supplements if your healthcare provider recommends it. Vitamin D and calcium work together. Ask your healthcare provider if it’s a good idea for you to take Vitamin D with a calcium supplement. What about Chromium, and Vitamins C and E? There are some studies showing that these nutrients might be helpful for blood glucose control or heart health, but more research is needed. News stories over the past few years have reported that chromium might decrease body fat and build muscle without you having to change your eating habits. But, studies have not shown that chromium helps you lose weight. Also, it is not known how much chromium you should take. Fortunately, it is relatively safe. In fact, many healthcare providers tell their patients with diabetes to take chromium supplements. However, don’t take a chromium supplement without first talking with your healthcare team and knowing the correct amount to take. You might damage your kidneys if you take too much chromium. Good food sources of chromium include whole grains, bran cereals, seafood, green beans, nuts, peanut butter, and potatoes. People with diabetes may have lower levels of vitamin C in their bodies. This may be because higher blood glucose levels keep vitamin C out of the body’s cells. In one study, people with type 2 diabetes who took 2,000 mg of Vitamin C every day showed improvement in blood glucose and fat levels. However, more studies need to be done to confirm the benefits for people with diabetes so ask your healthcare provider first before taking vitamin C supplements. Some studies say that vitamin E might help prevent health problems such as heart disease, eye problems and kidney damage. However, it’s too early to know if this is true. In addition, experts are not sure how much vitamin E you should take. Vitamin E amounts greater than 800 IU each chance of stroke in people with high blood pressure. Too much vitamin E can also keep medicines that prevent blood clots from working. If you want to take vitamin E, ask your healthcare provider first about the pros and cons and if you do decide to take vitamin E, do not take more than 200 Tips for Taking Supplements Pick supplements with no more than 100 to 150 percent of the daily value for the listed vitamins and minerals Women who have gone through menopause should choose a supplement without iron Choose a brand that has the USP seal on the package. A USP (U.S. Pharmacopeia) seal says the product has been tested for strength and purity Check expiration dates; do not use expired supplements Keep supplements in a cool, dry place, and out of reach of children.
The post Vitamins and Diabetes Care appeared first on Spring 2017 Issue | CDiabetes Online Magazine.
]]>
By Robert Ehrman, MD ? Reviewed by Fran Daniel, MPH
First, it is important to note that eating a variety of whole foods is a better choice for staying healthy than relying on vitamins or supplements.?Eating lean meats, vegetables, fruits, and whole grains- and limiting fats and sugar — are important for keeping your blood glucose under control.
Individual foods can give you many different vitamins, minerals, and nutrients, in one?serving. For example, raspberries contain vitamin C, fiber, and antioxidants. These nutrients, plus all?the food nutrients we have not yet discovered, work?together in your body to ensure that you benefit from all of them. Using vitamins or supplements – which do not have the full range of nutrients that whole foods do — may not?be needed unless you have a specific vitamin deficiency. (“Deficiency” means that your body does not have enough?of an important nutrient.) It’s a good idea to talk to your healthcare provider before taking any vitamin supplements to see if you really need them.
Your healthcare provider may want you to take?vitamin supplements if you are:
- On a low-calorie diet and do?not eat a wide variety of foods
- On a vegan diet (no meat, fish, eggs or dairy products)
- Pregnant
- On a restricted diet because you?have food allergies, kidney disease?or have trouble absorbing nutrients
What Vitamins Are The Best?
Many people, including those with diabetes, may?need to take vitamin D supplements.?Experts say to take 400 international units (IU) each day. Recent studies suggest that this may not be enough vitamin D. Ask your healthcare provider if you ?should take vitamin D supplements,?and how much to take every day.
Why Is Vitamin D So Important For Good Health?
Vitamin D might be able to:
- improve pain and tingling in your legs, feet, hands, and fingers.
- keep bones healthy and strong
- help with blood glucose control
- help ease depression in women with type 2 diabetes.
How Can I Get More Vitamin D?
-
Go outside in the sunshine. Sunshine is a great way to get vitamin D. To be safe, first check with your healthcare provider to make sure it’s safe for you to spend time in the sun.
- Eat more fish and egg yolks.
- Eat cereals with vitamin D added.
- Drink milk with vitamin D added.
- Take Vitamin D supplements if your healthcare provider recommends it.
- Vitamin D and calcium work together. Ask your healthcare provider if it’s a good idea for you to take Vitamin D with a calcium supplement.
What about Chromium, and Vitamins C and E?
There are some studies showing that these nutrients might be helpful for blood glucose control or heart health, but more research is needed. News stories over the past few years have reported that chromium might decrease body fat and build muscle without you having to change your eating habits. But, studies have not shown that chromium helps you lose weight. Also, it is not known how much chromium you should take. Fortunately, it is relatively safe. In fact, many healthcare providers tell their patients with diabetes to take chromium supplements. However, don’t take a chromium supplement without first talking with your healthcare team and knowing the correct amount to take. You might damage your kidneys if you take too much chromium. Good food sources of chromium include whole grains, bran cereals, seafood, green beans, nuts, peanut butter, and potatoes.
People with diabetes may have lower levels of vitamin C in their bodies. This may be because higher blood glucose levels keep vitamin C out of the body’s cells. In one study, people with type 2 diabetes who took 2,000 mg of Vitamin C every day showed improvement in blood glucose and fat levels. However, more studies need to be done to confirm the benefits for people with diabetes so ask your healthcare provider first before taking vitamin C supplements. Some studies say that vitamin E might help prevent health problems such as heart disease, eye problems and kidney damage. However, it’s too early to know if this is true. In addition, experts are not sure how much vitamin E you should take. Vitamin E amounts greater than 800 IU each chance of stroke in people with high blood pressure. Too much vitamin E can also keep medicines that prevent blood clots from working. If you want to take vitamin E, ask your healthcare provider first about the pros and cons and if you do decide to take vitamin E, do not take more than 200
Tips for Taking Supplements
- Pick supplements with no more than 100 to 150 percent of the daily value for the listed vitamins and minerals
- Women who have gone through menopause should choose a supplement without iron
- Choose a brand that has the USP seal on the package. A USP (U.S. Pharmacopeia) seal says the product has been tested for strength and purity
- Check expiration dates; do not use expired supplements
- Keep supplements in a cool, dry place, and out of reach of children.
The post Vitamins and Diabetes Care appeared first on Spring 2017 Issue | CDiabetes Online Magazine.
]]>
By Martha Funnell, MS, RN, CDE For most women, the idea of starting a family is both exciting and scary. It is exciting to think how you can create a new life and perhaps have a dream come true. It can also be a time of worry as you think about how your life will change. Women who have diabetes may also worry about how diabetes can affect their pregnancy and their future child. The good news is that more and more women with both type 1 and type 2 diabetes are having safe pregnancies and healthy babies than ever before. As you might expect, it takes more planning and more work, but the results are worth it. PRE-PREGNANCY First, visit with your health care provider before you get pregnant. During this visit, you and your provider will talk about your general health, diabetes treatment and current blood glucose levels. You may have your eyes and kidneys checked for signs of damage. If you take insulin, the dose and types of insulin you take may be changed. If you take diabetes pills, you may need to switch the types you take or start insulin during your pregnancy. Think of this as the time to get your body ready to nurture a new life in the best possible way. It is best to keep your A1C level close to normal before you try to get pregnant. Because a baby’s organs are formed very early during pregnancy, birth defects can occur if blood glucose levels are too high. If you get and keep your blood glucose levels in your target range, it will give your baby a good start. The other thing that you can do before you become pregnant is to take folic acid. This can help prevent birth defects. Your health care provider can offer advice about how much to take and when to start. This is also a good time to change health habits that you have been putting off. Do you want to eat better foods, move more, become more active or stop smoking? Now is a great time to start. When you struggle to stick with your plan, picture yourself holding your new baby. What could be more motivating than that? PREGNANCY The goal for diabetes care during pregnancy is to keep your blood glucose as close to normal as possible. As your need for insulin rises, your medicines will likely change. If you did not take insulin before pregnancy, you may need it until you deliver. If you were taking insulin, the types and doses may change. To keep your blood glucose in this very tight range, you will also need to watch your control more closely, pay close attention to your food, activity and stress levels, and see your health care team often. You and your baby will be watched very carefully during your entire pregnancy. Although having these tests may be scary, it is the best way to be sure that you and your baby are both doing well. DELIVERY Women with diabetes can have normal births, although your chances of having induced labor or a Caesarean section are increased. Women with diabetes are more likely to have a large baby if their blood glucose levels are high near the end of pregnancy. During the birth of your baby, your progress will be watched very closely to be sure that all is well. After the baby is born, he or she will be checked often. The baby’s blood glucose level will be checked for a low blood glucose level, which is not the same as diabetes. Low blood glucose can occur because the baby has been making extra insulin to be sure that his or her blood glucose stays in the normal range. Once the baby is born, it may take a day or two to adjust. Finally, your baby is here and you are ready to go home. There is no question that you will work harder than other women during your pregnancy, but there is also no question that a new life is well worth all of your efforts.
The post Expecting To Be Expecting? appeared first on Spring 2017 Issue | CDiabetes Online Magazine.
]]>
The post Expecting To Be Expecting? appeared first on Spring 2017 Issue | CDiabetes Online Magazine.
]]>
The post Nature Made? Vitamins appeared first on Spring 2017 Issue | CDiabetes Online Magazine.
]]>
The post Nature Made? Vitamins appeared first on Spring 2017 Issue | CDiabetes Online Magazine.
]]>
By Martha Funnell, MS, RN, CDE Has this ever happened to you: You are using your meal plan and keeping your blood glucose levels in the target range. Just when you feel you have it all under control, something happens to stress you out. Almost without thinking, you reach for your favorite comfort food. You feel better for a while, but then your blood glucose levels go up. So now you feel tired, guilty and even more stressed. You can break this stress-eating cycle. Instead of getting down on yourself or thinking there is nothing you can do to change, you can learn to handle stress in a new way. FOOD AND STRESS There is nothing wrong with eating during times of stress—the problem is what you eat. Most people don’t choose carrots and celery as a way to ease stress. It’s much more likely that you’ll reach for comfort foods that are often high in carbs, fat and calories, such as potato chips, cookies and ice cream. The foods that you find comforting often go back many years, maybe even to childhood. It can be a tough cycle to break, but by learning more about yourself and making a plan, you can do it. DID IT HELP? The first thing to do is to think about why you use food and how well it is working for you. Think back to when you last ate due to stress. Many people find that food is only a short-term solution. It does not really fix the problem or make the stress go away. In fact, you may feel more stressed. One idea is to avoid people or things that are stressful as often as you can. It takes time to feel good about saying “No,” but it may help to remember that it is in your best interest. And you will be more help to others if you are in better health. But even if you can’t get rid of or control the things you find stressful, you do have a choice about how you handle it. MAKE A PLAN One of the reasons people eat when they are stressed is that comfort foods are often not part of their daily meal plan. They end up craving those foods and during stressful times, they reach for them because they feel they deserve it. A way to lessen those cravings is to have small portions of comfort foods routinely so they are less of a treat. A dietitian can help you learn how to fit favorite foods into your meal plan. There are lots of tips for handling stress, but it can be hard to remember these ideas when you are in the middle of a tough situation. One thought is to make a plan when you are not stressed. Being ready for stress with a list of things you know will work or want to try can make it easier to use these tips when you need them. Think of it as reaching for your list instead of a cookie. Stress is part of life. So having a plan in place just makes sense. It can help you break the stress-eating cycle and help you feel more in charge of your diabetes and your life. ASK YOURSELF ? Did eating help? ? Did I feel better or worse? ? If I felt better, for how long? ? Did eating cause additional stress or make it go away? ? What could I do instead? 7 TIPS FOR MANAGING STRESS 1 Avoid or get rid of what’s causing it. 2 Change your belief about it. 3 Learn new ways to deal with it. 4 Take a walk. 5 Talk with a good listener. 6 Write down your feelings. 7 Pray and/or meditate.
The post Break The Stress-Eating Cycle appeared first on Spring 2017 Issue | CDiabetes Online Magazine.
]]>
The post Break The Stress-Eating Cycle appeared first on Spring 2017 Issue | CDiabetes Online Magazine.
]]>
Available only at Costco Wholesale Outlets
The post Sunmark? Brand Products appeared first on Spring 2017 Issue | CDiabetes Online Magazine.
]]>

The post Sunmark? Brand Products appeared first on Spring 2017 Issue | CDiabetes Online Magazine.
]]>
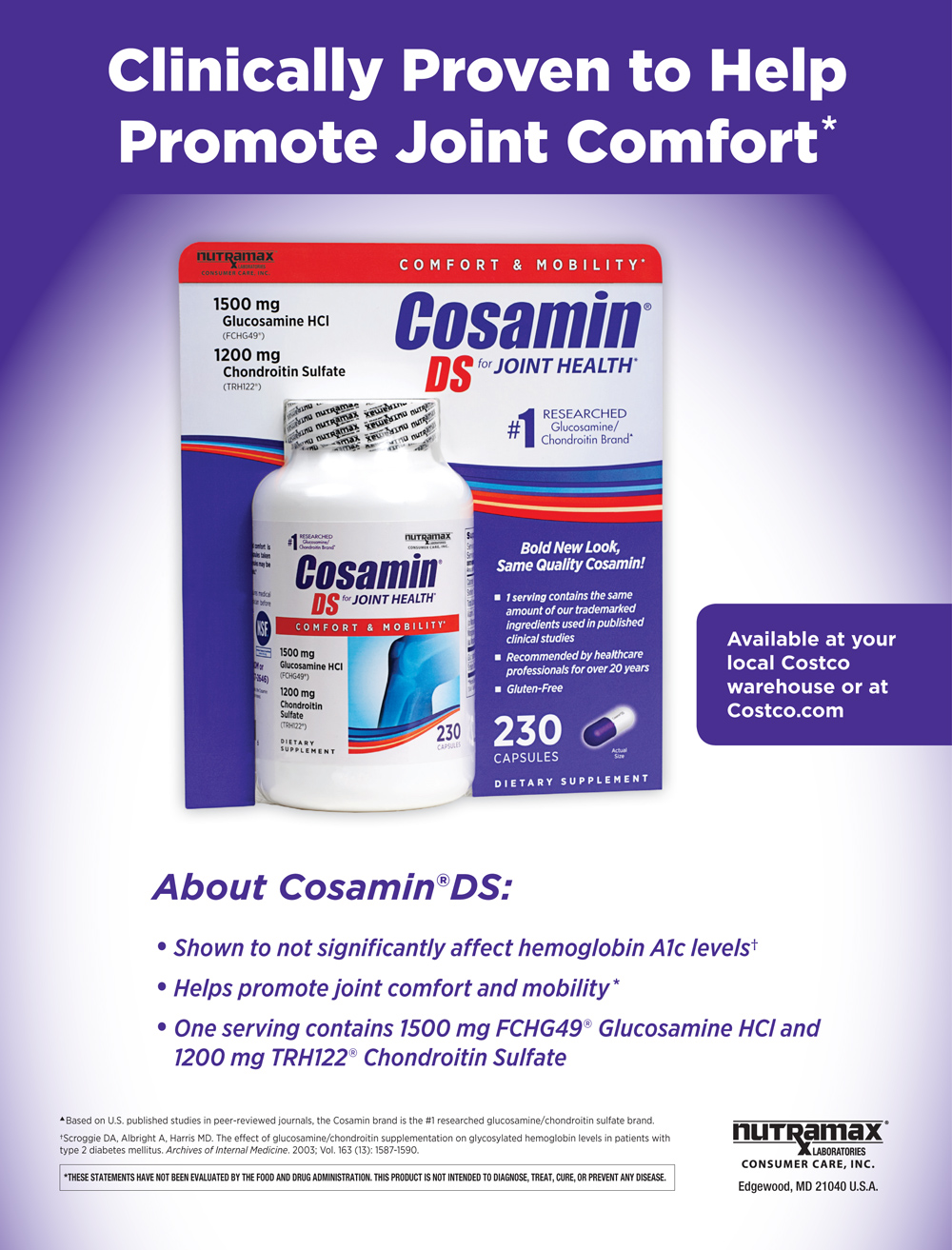
The post Cosamin ? DS for Joint Health appeared first on Spring 2017 Issue | CDiabetes Online Magazine.
]]>
The post Cosamin ? DS for Joint Health appeared first on Spring 2017 Issue | CDiabetes Online Magazine.
]]>
By Holly Clegg Corn chowder packed with fabulous flavors and good nutrition; all in one bowl. Makes 8 (1-cup) servings 2 tablespoons olive oil 1 onion, diced 1 cup chopped celery 1 teaspoon minced garlic 1/4 cup all-purpose flour 2 cups skim milk 2 cups low sodium fat-free vegetable or chicken broth 1 (16-ounce) package frozen corn 1 large Louisiana yam (sweet potato), peeled and cut into 1/2 inch cubes Salt and pepper to taste 1 1/2 cups chopped kale Directions In large nonstick pot, heat oil and sauté onion, celery and garlic until tender, 5-7 minutes. Whisk in flour and cook, stirring constantly one minute. Gradually add milk and broth; bring to boil, stirring several minutes or until mixture thickens. Lower heat and add corn and sweet potato, cooking until sweet potato is tender, 6-8 minutes. Season to taste. Before serving stir in kale, cooking several minutes. NUTRITION INFORMATION PER SERVING: Calories 186 Calories from Fat 18% Fat 4g Saturated Fat 1g Cholesterol 1mg Sodium 91mg Carbohydrates 34g Dietary Fiber 4g Total Sugars 9g Protein 6g Dietary Exchanges: 2 starch, 1 vegetable, 1/2 fat Terrific Tip: If you want the soup a little thicker, dissolve two teaspoons cornstarch in a little water and add. After refrigerating leftovers, if too thick, add more broth.
The post Chunky Corn Chowder With Kale And Sweet Potato appeared first on Spring 2017 Issue | CDiabetes Online Magazine.
]]>
The post Chunky Corn Chowder With Kale And Sweet Potato appeared first on Spring 2017 Issue | CDiabetes Online Magazine.
]]>
By Holly Clegg Simple seasonings perk up salmon with a sweet and spicy rub. Easy to make and oh-so enjoyable to eat. Makes 4 servings 2 tablespoons light brown sugar 4 teaspoons chili powder 1 teaspoon ground cumin 1/4 teaspoon ground cinnamon Salt and pepper to taste 4 (6-ounce) salmon fillets Directions Preheat oven 400°F. Coat 11x7x2-inch baking dish coated with nonstick cooking spray. In small bowl, mix together brown sugar, chili powder, cumin, cinnamon and season to taste. Rub over salmon and place in prepared Bake 12 - 15 minutes or until fish flakes easily when tested with fork. NUTRITION INFORMATION PER SERVING: Calories 257 Calories from Fat 29% Fat 8g Saturated Fat 1g Cholesterol 80mg Sodium 177mg Carbohydrates 8g Dietary Fiber 1g Total Sugars 7g Protein 36g Dietary Exchanges: 1/2 other carbohydrate, 5 lean meat Nutritional Nugget: At least two servings of fish ( fatty fish preferred) per week is the recommended intake by the American Heart Association.
The post Roasted Seasoned Salmon appeared first on Spring 2017 Issue | CDiabetes Online Magazine.
]]>
The post Roasted Seasoned Salmon appeared first on Spring 2017 Issue | CDiabetes Online Magazine.
]]>
By Holly Clegg Fresh unassuming Brussels sprouts pop with flavor and freshness. Makes 4 servings 1 pound Brussels sprouts 2 tablespoons olive oil 1 teaspoon minced garlic 3 tablespoons lemon juice Salt and pepper to taste Directions Cut ends off Brussels sprouts and slice in half. In medium nonstick skillet, heat olive oil and when hot, add halved Brussels sprouts, stirring, 6-8 minutes, or until caramelized brown and tender. Add garlic when almost done. When done, reduce heat and add lemon juice; season to taste. NUTRITION INFORMATION PER SERVING: Calories 112 Calories from Fat 52%Fat 7gSaturated Fat 1gCholesterol 0mg Sodium 29mgCarbohydrates 11g Dietary Fiber 4g Total Sugars 3gProtein 4g Dietary Exchanges: 2 vegetable, 1 1/2 fat Nutrition Nuggets: Brussels sprouts high levels of vitamin C help collagen production and important for healthy tissues and organs.
The post Lemon Garlic Brussels Sprouts appeared first on Spring 2017 Issue | CDiabetes Online Magazine.
]]>
The post Lemon Garlic Brussels Sprouts appeared first on Spring 2017 Issue | CDiabetes Online Magazine.
]]>
By Holly Clegg These tasty squares may be served hot, at room temperature, or even out of the refrigerator—just cover when reheating. Makes 30 squares 1 cup chopped onion 1 cup chopped red bell pepper 1 cup chopped green bell pepper 1 cup sliced mushrooms 1 teaspoon minced garlic 2 (14-ounce) cans artichoke hearts, drained, rinsed, and chopped 3 egg whites, slightly beaten 2 eggs, slightly beaten 1 teaspoon dried oregano leaves 1 teaspoon dried basil leaves 1/4 teaspoon Cayenne pepper 1/2 cup Italian bread crumbs 3/4 cup shredded reduced-fat sharp Cheddar cheese 1/4 cup grated Parmesan cheese Directions Preheat oven 350°F. Coat 2-quart oblong dish with nonstick cooking spray. In medium pan coated with nonstick cooking spray, sauté onion, red and green pepper, mushrooms, and garlic over medium heat until tender. Transfer sautéed vegetables into large bowl, add chopped artichokes and remaining ingredients, stirring until combined. Pour mixture into prepared dish. Bake 30 minutes or until mixture is set and top is light brown. Cut into squares. NUTRITION INFORMATION PER SERVING: Calories 37Calories from Fat 28%Fat 1gSaturated Fat 1gCholesterol 16mgSodium 119mgCarbohydrates 4g Dietary Fiber 1gSugar 1gProtein 3g Dietary Exchanges: 1 vegetable Nutrition Nugget: Artichokes are a naturally low-sodium, fat-free, low calorie food, rich in healthy antioxidants and phytonutrients.
The post Artichoke Squares appeared first on Spring 2017 Issue | CDiabetes Online Magazine.
]]>
The post Artichoke Squares appeared first on Spring 2017 Issue | CDiabetes Online Magazine.
]]>
By Janis Roszler MSFT, RD, CDE, LD/N Diabetes and food do a unique dance. You need to eat a variety of foods to stay healthy, but too much of some foods can lead to weight gain and can affect your diabetes control. Your diabetes food plan should fit your nutritional needs, daily routine, eating habits, food likes, and blood glucose and diabetes goals. You and your diabetes care team should find the method that best helps you plan meals, stay healthy, and maintain proper weight and blood fat (lipid) goals. And if one approach doesn’t work for you, try another. There are many diabetes meal planning methods to choose from. Which one is best for you? Here are three popular methods ?to consider. 1. The Plate Method This simple meal planning method is easy to use at home and when you eat out. For breakfast Draw a pretend line down the middle of your 9-inch plate. Place a small carbohydrate serving of whole-grain toast or cereal on one side. Split the other half of the plate into two sections. Fill one with a meat or meat substitute, such as an egg, egg whites, low-fat cottage cheese or Canadian bacon. Fill the other part with a small piece of fruit or enjoy ? cup of juice. If you wish, you can also have a cup of skim or low-fat milk, sugar-free hot chocolate or light yogurt. If you use a bowl at breakfast, keep your portions small. For lunch and dinner Again, draw a pretend line down the middle of a 9-inch plate. Fill one side with non-starchy (low-carb) vegetables, such as green beans, zucchini, cauliflower, spinach, summer squash, Brussels sprouts, carrots, broccoli, peppers, tomatoes, cucumbers, celery and lettuce. Then, split the other side into two equal parts. Fill one part with carbohydrate-rich foods, such as baked or sweet potato, corn, peas, chickpeas, lentils, kidney beans, or whole-grain rice, pasta or bread. The last part of your plate should be filled with protein foods, such as skinless chicken or turkey, fish, eggs, lean beef or pork, low-fat cheese, low-fat cottage cheese or tofu. To round out your meal, add a small fruit serving (? cup or one small piece of fruit) and 8 ounces of skim or low-fat milk or 1 cup of light yogurt. 2. Carb Counting When you know how many carbohydrates (carbs) are in each serving of food, you ?can eat the amount that will help you maintain good glucose control. Foods that have carbohydrates will raise your blood glucose level. Experts suggest that people with diabetes eat at least 130 grams of carbohydrates each day to stay healthy. Many people eat 45–60 grams of carbs at each meal and 10–15 grams for each snack. A dietitian can help you use this method to plan your meals. If you use insulin, your dietitian can also help you use your carbohydrate totals to figure out how much insulin to take at mealtimes. 3. Glycemic Index This tool can help you get the most out of your diabetes meal plan. The Glycemic Index (GI) ranks carbohydrate foods by the effect they have on the body’s glucose level. Foods are listed as having a high, medium or low GI. Low foods have the smallest effect and high foods have the greatest. The list is not perfect but can help you make better food choices when you plan your meals. For example, if you want to eat a fruit but don’t want your glucose level to jump too high, choose one that has a low or medium GI. These meal-planning methods offer you ways to eat well while at home and away. Meet with a dietitian to learn the best way to use them.
The post Diabetes Meal Planning: Which Method is Best for You? appeared first on Spring 2017 Issue | CDiabetes Online Magazine.
]]>
By Janis Roszler MSFT, RD, CDE, LD/N
Diabetes and food do a unique dance. You need to eat a variety of foods to stay healthy, but too much of some foods can lead to weight gain and can affect your diabetes control. Your diabetes food plan should fit your nutritional needs, daily routine, eating habits, food likes, and blood glucose and diabetes goals. You and your diabetes care team should find the method that best helps you plan meals, stay healthy, and maintain proper weight and blood fat (lipid) goals. And if one approach doesn’t work for you, try another.
There are many diabetes meal planning methods to choose from. Which one is best for you? Here are three popular methods ?to consider.
1. The Plate Method
This simple meal planning method is easy to use at home and when you eat out.
For breakfast
Draw a pretend line down the middle of your 9-inch plate. Place a small carbohydrate serving of whole-grain toast or cereal on one side. Split the other half of the plate into two sections. Fill one with a meat or meat substitute, such as an egg, egg whites, low-fat cottage cheese or Canadian bacon. Fill the other part with a small piece of fruit or enjoy ? cup of juice. If you wish, you can also have a cup of skim or low-fat milk, sugar-free hot chocolate or light yogurt. If you use a bowl at breakfast, keep your portions small.
For lunch and dinner
Again, draw a pretend line down the middle of a 9-inch plate. Fill one side with non-starchy (low-carb) vegetables, such as green beans, zucchini, cauliflower, spinach, summer squash, Brussels sprouts, carrots, broccoli, peppers, tomatoes, cucumbers, celery and lettuce. Then, split the other side into two equal parts. Fill one part with carbohydrate-rich foods, such as baked or sweet potato, corn, peas, chickpeas, lentils, kidney beans, or whole-grain rice, pasta or bread. The last part of your plate should be filled with protein foods, such as skinless chicken or turkey, fish, eggs, lean beef or pork, low-fat cheese, low-fat cottage cheese or tofu. To round out your meal, add a small fruit serving (? cup or one small piece of fruit) and 8 ounces of skim or low-fat milk or 1 cup of light yogurt.
2. Carb Counting
When you know how many carbohydrates (carbs) are in each serving of food, you ?can eat the amount that will help you maintain good glucose control.
Foods that have carbohydrates will raise your blood glucose level. Experts suggest that people with diabetes eat at least 130 grams of carbohydrates each day to stay healthy. Many people eat 45–60 grams of carbs at each meal and 10–15 grams for each snack. A dietitian can help you use this method to plan your meals. If you use insulin, your dietitian can also help you use your carbohydrate totals to figure out how much insulin to take at mealtimes.
3. Glycemic Index
This tool can help you get the most out of your diabetes meal plan.
The Glycemic Index (GI) ranks carbohydrate foods by the effect they have on the body’s glucose level. Foods are listed as having a high, medium or low GI. Low foods have the smallest effect and high foods have the greatest. The list is not perfect but can help you make better food choices when you plan your meals. For example, if you want to eat a fruit but don’t want your glucose level to jump too high, choose one that has a low or medium GI.
These meal-planning methods offer you ways to eat well while at home and away. Meet with a dietitian to learn the best way to use them.
The post Diabetes Meal Planning: Which Method is Best for You? appeared first on Spring 2017 Issue | CDiabetes Online Magazine.
]]>
By Janis Roszler, RD, CDE, LD/N When you were young, did your mother tell you not to eat between meals? Many people still think snacking is a no-no. They worry that the snacks they eat will cause them to gain weight and become less healthy. But experts who reviewed the eating habits of more than 11,000 people found that many of the snackers were very healthy eaters. They tended to drink more milk, eat more fruit and whole grains and consume less sodium in general. And the biggest surprise of all? The more they snacked, the better they ate overall. BECOME A “SNACKER” While not everyone with diabetes chooses or needs to eat them, there are many great reasons to enjoy healthy between-meal snacks each day. A snack helps you keep your energy level up and blood glucose levels from dropping too low. Blood glucose levels tend to dip a few hours after a meal, and this can cause your energy level to drop. A well-timed, healthy snack can help you keep your engine roaring. Some snacks make you happier. If your snack contains carbohydrates, it will raise your brain’s serotonin level, which helps improve your mood. A snack helps you feel less hungry. When your next mealtime rolls around, you may be less tempted to overeat. A snack helps you say no. If you carry healthy snacks with you, you may have an easier time saying no to a vending machine treat or tempting office dessert. A snack helps you maintain your energy. Eat a snack before your workout, for example, to help keep your energy level up and prevent your blood glucose level from going too low. A snack helps you feel less deprived. It sure feels better to say yes to a healthy snack choice than no to a high-calorie, high-fat treat. FIND GOOD SNACKS If you have diabetes, a low-carb or carbohydrate-free snack is a great choice. Many people with diabetes limit their snack choices to foods that contain 15 or fewer grams of carbohydrates. Snacks with 15 or fewer grams of carbs per serving tend not to raise your blood glucose level by much. Some people also find that eating a small amount of protein or healthy fat along with their snack, such as a small piece of low-fat cheese or a few nuts, helps keep them full. When you pick your snacks, stay away from unhealthy fried foods, trans-fats (check the Nutrition Facts label) and high-calorie desserts. Keep your portion small and don’t go back for a second helping. A great way to stretch your snack is to enjoy it with water or a flavored, calorie-free drink. BEST TIMES TO SNACK Think about your day and note the times when you start to feel hungry or have a drop in energy between meals. Those are possible snack times. If you eat your snack just before your energy drop occurs, you may be able to prevent the drop from happening. If you want to lose weight, limit the size of your snacks. If they are too large, you may gain weight over time. A snack is not a small meal: It is a nibble that helps you make it to your next meal. Meet with a registered dietitian to learn how to add snacks to your current meal plan. Prepare for the snack attack and go for it. SNACKS WITH 15 GRAMS OF CARBOHYDRATES OR FEWER ? Nuts (no more than a handful—they are high in calories) ? A hard-boiled egg ? Low-fat cheese ? Cut-up vegetables with low-fat dressing ? 1 cup sugar-free hot chocolate ? Low-fat turkey or chicken cold cuts ? 1 medium-sized fruit ? 1 low-carb snack bar ? Pickles ? 3/4 cup of light, no-sugar-added or plain yogurt ? 10 baked potato chips ? 5 vanilla wafers ? 3 cups of plain popcorn ? 2 ounces of canned fish (tuna) with light mayonnaise ? Celery with light cheese spread
The post Snack Attack appeared first on Spring 2017 Issue | CDiabetes Online Magazine.
]]>
The post Snack Attack appeared first on Spring 2017 Issue | CDiabetes Online Magazine.
]]>
By Martha Funnell, MS, RN, CDE One of the hardest things about living with diabetes is thinking about the possibility of long-term complications: eye, kidney and nerve damage, as well as heart attacks and strokes. You may already know that keeping your blood glucose as close to normal as is safe for you is the best way to lower your risk. The target for most people with diabetes is to keep their A1C levels at less than 7%. But here are some other steps you can take to lower your risk for these complications. HIGH BLOOD PRESSURE Having high blood pressure along with diabetes increases your risk of complications. High blood pressure increases the force of the blood through your blood vessels. Over time, that can damage both the small blood vessels and the large blood vessels. Damage to the small blood vessels in your eyes and kidneys increases your risk of eye disease and kidney damage. Damage to the large blood vessels increases your risk of heart attacks and strokes. Two blood pressure medicines commonly used for people with diabetes are ACE inhibitors, or ARBs. These medicines not only lower your blood pressure but also help protect your kidneys. Even when your blood pressure reaches the target range, taking your medicines helps to keep it there. That is why it is important for you to continue taking your medicines for high blood pressure, even if your blood pressure is within your target range. 130/80 The recommended target for blood pressure among people with diabetes is 130/80 mmHg or lower. STRESS Stress can raise both your blood glucose and your blood pressure. You cannot always control the amount of stress in your life, but you can learn to handle it differently. Physical activity, meditation, prayer, yoga and relaxation exercises are all positive ways to deal with stress. Another idea is to avoid, as much as you can, events that cause you to feel stressed. Or try a support group for people with diabetes. SMOKING Smoking is not good for anyone, but it is more harmful for people with diabetes. When you smoke and have diabetes, you increase your risk for kidney and nerve damage. Smoking also damages the heart and blood vessels and adds greatly to your risk for heart attack and strokes. Wanting to prevent complications from diabetes is another good reason to stop smoking. If you do smoke, try to cut down on the amount you smoke. Talk with your healthcare team about ways to stop smoking. Medicines, nicotine patches or gum and/or stop-smoking programs or help lines can all help. IMPROVE BLOOD GLUCOSE AND BLOOD PRESSURE Fortunately, many of the things you do to lower your blood glucose also help to lower your blood pressure. These include weight loss, physical activity and eating more vegetables, fruits and whole grains. Less salt in your diet may also help lower your blood pressure. ALCOHOL Drinking too much is especially unhealthy for people with diabetes. Alcohol is high in calories, low in food value and can get in the way of your exercise and weight loss goals. Too much alcohol can damage your heart, blood vessels and liver. Talk with your healthcare provider if you believe you are drinking too much or if you want to stop. He or she can tell you about resources in your area. Lowering your risk for complications is the main goal of managing diabetes. Going beyond blood glucose gives you the greatest chance for living a longer, healthier life. It is a lot to do and it isn’t always easy, but most people find that it is worth the effort.
The post Beyond Blood Glucose appeared first on Spring 2017 Issue | CDiabetes Online Magazine.
]]>
The post Beyond Blood Glucose appeared first on Spring 2017 Issue | CDiabetes Online Magazine.
]]>


![tn_CinSulin_ad_2016[4x5]](http://www.keixun.com.cn/spring2017/wp-content/uploads/2016/01/tn_CinSulinVitBest_DigitalMay2017-400.jpg)
![tn_CinSulin_ad_2016[4x5]](http://www.keixun.com.cn/spring2017/wp-content/uploads/2016/01/tn_CinSulinVitBest_DigitalMay2017-1000.jpg)