You and your family can work together to create a road map to lower your risks for diabetes, health disease and other health problems. First, the not-so-good news: Type 2 diabetes runs in families. This means that if you have diabetes, your children, grandchildren, brothers and sisters are all at risk. Now, here is the good news: As the National Diabetes Education Program points out, you can’t change your genes, but you can change your future— and you can help your family members change their futures as well. Preventing Diabetes A large study was done several years ago called The Diabetes Prevention Program (DPP). The study looked at over 3,000 people with higher than normal blood glucose levels. While their levels were not high enough to cause them to be diagnosed with diabetes, they did show that those people had a condition called prediabetes. Almost half of the people in the study were members of racial groups with high rates of type 2 diabetes: African-Americans, Hispanic-Americans, Asian-Americans, Pacific Islanders and American Indians. The study also included other groups of people at higher risk for type 2 diabetes, such as people aged 60 and over, women with a history of ?diabetes during pregnancy, and people with a parent, sibling or other relative with type 2 diabetes. The goal of the study was to see what people can do to help prevent the onset of diabetes. Of the people who took part in the study, one group reduced its risk for getting Type 2 diabetes by 58%. On average, this group exercised a total of 30 minutes per day, usually by walking or another moderate activity. They also lost 5% to 7% of their body weight, an average of 15 pounds. 1 UNDERSTAND THE RISKS Your family members need to know that you have diabetes so they can understand their own risk for diabetes. Although it is tempting not to tell them so that you can keep them from worrying, they need to know so that they can take their risk seriously. Some people use the chance to tell family members as a way to start talking about what they are doing to take care of their diabetes. Let them know that you are telling them about your condition because you care about them and want to help them be healthier. We know that people with diabetes are better able to manage their condition and their feelings about it when they have the love, support and understanding of their family and friends. 2 MAKE A PLAN Ask your family members to help you make a plan for managing your diabetes. Then talk about how you can help them to take steps to eat healthier and be more active. This way, you are both supporting each other in having healthy lifestyle plans. For example, you may talk about how to have healthier choices on the menu when you all get together for a meal. If you live close to one another, you may decide to walk or do other kinds of exercise together. Knowing that you are all working toward a common goal can bring your family closer. Supporting each other helps everyone to succeed. 3 INCLUDE YOUR CHILDREN Include children and grandchildren in your planning. The number of young people with type 2 diabetes is growing rapidly. Together, come up with a plan to keep them active and at a healthy weight. Turning off the TV, iPad, computer and cell phone and taking a walk or going to the park are good ways to connect and be active at the same time. 4 COMMUNITY INVOLVEMENT Think about ways you can involve your community, place of worship or school in diabetes prevention efforts. Support groups, walking clubs and community gardens are great ways to bring the neighborhood together. Encouraging healthier choices in the school cafeteria and other events where food is served will help everyone. Managing diabetes is not always easy but it is worth the effort. The same is true for lowering your risk for diabetes. Making a plan and providing and receiving support can help every person to be more successful. Getting more active and losing weight helped all age and ethnic groups, but it was especially helpful for the elder group. They reduced their risk for diabetes by 71% with these lifestyle changes. Another way to prevent diabetes is with medication. A different group that took part in the study was given metformin, a pill that is used to treat diabetes. People in the group that took metformin reduced their risk of getting Type 2 diabetes by about one-third. This medicine worked better in people who were younger and very overweight. ? ? ? Type 2 diabetes tends to run in families. Despite what you may have heard, diabetes does not “skip a generation.” You are more likely to get ?diabetes if your father or mother had it. By Martha Funnell, MS, RN, CDE
The post Keeping Healthy is a Family Affair appeared first on Spring 2016 Issue | CDiabetes Online Magazine.
]]>
The post Keeping Healthy is a Family Affair appeared first on Spring 2016 Issue | CDiabetes Online Magazine.
]]>
If you have diabetes, you probably know that you are at an increased risk for problems with your eyes, feet, skin?and nervous system. Did you know that diabetes can also cause problems in your mouth? Take Care Of Your Teeth Poor blood glucose control lets bacteria grow easily in your mouth. Having lots of bacteria in your mouth lead to?plaque buildup on your teeth. When this happens, your gums begin to pull away from your teeth, and pockets form between your teeth and gums. These pockets can become filled with germs and small bits of food. The gums then become inflamed and may bleed when you eat or brush your teeth. This condition is called “gingivitis”. Keeping your gums healthy is important because they help to hold your teeth in place. If nothing is done, you can get an infection in your gums that can go on to destroy the bone around your teeth, and they may start to move. Your teeth may fall out or need to be pulled. A recent study at the University of Copenhagen in Denmark looked at the link between oral health and diabetes. The study found that people with good oral health practices, along with a healthy diet and good stress management, had?lower blood glucose levels and healthier teeth and gums. Diabetes: A Major Cause Of Gum Disease There are many causes of gum disease, including smoking, hormonal changes, and certain cancers. Some medicines can?make your mouth dry, which can increase your risk for tooth and gum problems. This is because saliva helps slow the growth of bacteria and keeps your mouth healthy overall. Poorly controlled diabetes can also lead to gum disease. High levels of sugar in saliva make it easy for bacteria to grow there. This is why poorly controlled diabetes is a risk factor for gum disease. Also, diabetes can cause problems with blood flow to your teeth and gums. This makes it harder to repair damage to your gums and fight infection. It is also important to understand that if you develop gum disease from poor oral habits or other reasons, this could make it harder for you to control your diabetes. Other oral problems related to diabetes include: Thrush: this is an infection caused by a fungus that grows in the mouth and throat Dry mouth: this can cause soreness, ulcers, infections and cavities Dental Check-ups Are Important It’s important that you tell your dentist if you have diabetes, and keep them informed of any changes in your condition or medicines. Postpone any non-emergency dental procedures if your blood sugar is not well controlled. What Can You Do To Keep Your Mouth Healthy? The most important thing you can do is control your blood glucose levels. Have dental check-ups every six months?if possible. Avoid smoking and, if you wear dentures, remove and clean them every day. Good blood glucose control can also help prevent or relieve the dry mouth diabetes can cause. Here are some simple tips for a healthy mouth: Keep your blood glucose level under control Brush and floss every day Visit your dentist at least every 6 months. Be sure to tell them that you have diabetes Tell your dentist if your dentures do not fit right, or if your gums are sore Stop smoking. Your healthcare provider or dentist can tell you about what options there are to help you quit Call your dentist if you notice a problem. Take time to check your mouth regularly for any problems. If your gums bleed when you brush or floss, or if you notice dryness, soreness, white patches, or a bad taste in your mouth, contact your dentist right away. Remember, good blood glucose control can help keep your mouth happy and healthy for years to come. 6 Signs Of Gum Disease Red or swollen gums Gums that bleed easily when brushing or flossing Receding gums (pulling away from teeth) Loose teeth, making it hard to bite and chew Constant bad breath Dentures that don’t fit anymore By Robert Ehrman, MD
The post Oral Health And Diabetes appeared first on Spring 2016 Issue | CDiabetes Online Magazine.
]]>
If you have diabetes, you probably know that you are at an increased risk for problems with your eyes, feet, skin?and nervous system. Did you know that diabetes can also cause problems in your mouth?
Take Care Of Your Teeth
Poor blood glucose control lets bacteria grow easily in your mouth. Having lots of bacteria in your mouth lead to?plaque buildup on your teeth. When this happens, your gums begin to pull away from your teeth, and pockets form between your teeth and gums. These pockets can become filled with germs and small bits of food. The gums then become inflamed and may bleed when you eat or brush your teeth. This condition is called “gingivitis”.
Keeping your gums healthy is important because they help to hold your teeth in place. If nothing is done, you can get an infection in your gums that can go on to destroy the bone around your teeth, and they may start to move. Your teeth may fall out or need to be pulled.
A recent study at the University of Copenhagen in Denmark looked at the link between oral health and diabetes. The study found that people with good oral health practices, along with a healthy diet and good stress management, had?lower blood glucose levels and healthier teeth and gums.
Diabetes: A Major Cause Of Gum Disease
There are many causes of gum disease, including smoking, hormonal changes, and certain cancers. Some medicines can?make your mouth dry, which can increase your risk for tooth and gum problems. This is because saliva helps slow the growth of bacteria and keeps your mouth healthy overall. Poorly controlled diabetes can also lead to gum disease.
High levels of sugar in saliva make it easy for bacteria to grow there. This is why poorly controlled diabetes is a risk factor for gum disease. Also, diabetes can cause problems with blood flow to your teeth and gums. This makes it harder to repair damage to your gums and fight infection. It is also important to understand that if you develop gum disease from poor oral habits or other reasons, this could make it harder for you to control your diabetes.
Other oral problems related to diabetes include:
- Thrush: this is an infection caused by a fungus that grows in the mouth and throat
- Dry mouth: this can cause soreness, ulcers, infections and cavities
Dental Check-ups Are Important
It’s important that you tell your dentist if you have diabetes, and keep them informed of any changes in your condition or medicines. Postpone any non-emergency dental procedures if your blood sugar is not well controlled.
What Can You Do To Keep Your Mouth Healthy?
The most important thing you can do is control your blood glucose levels. Have dental check-ups every six months?if possible. Avoid smoking and, if you wear dentures, remove and clean them every day. Good blood glucose control can also help prevent or relieve the dry mouth diabetes can cause.
Here are some simple tips for a healthy mouth:
- Keep your blood glucose level under control
- Brush and floss every day
- Visit your dentist at least every 6 months. Be sure to tell them that you have diabetes
- Tell your dentist if your dentures do not fit right, or if your gums are sore
- Stop smoking. Your healthcare provider or dentist can tell you about what options there are to help you quit
- Call your dentist if you notice a problem.
Take time to check your mouth regularly for any problems. If your gums bleed when you brush or floss, or if you notice dryness, soreness, white patches, or a bad taste in your mouth, contact your dentist right away. Remember, good blood glucose control can help keep your mouth happy and healthy for years to come.
6 Signs Of Gum Disease
- Red or swollen gums
- Gums that bleed easily when brushing or flossing
- Receding gums (pulling away from teeth)
- Loose teeth, making it hard to bite and chew
- Constant bad breath
- Dentures that don’t fit anymore
By Robert Ehrman, MD
The post Oral Health And Diabetes appeared first on Spring 2016 Issue | CDiabetes Online Magazine.
]]>
Most of us don’t think about our feet very often, but they are certainly one of the most abused parts of the body. and if there is a problem, painful feet can really make your life miserable. how many times have you heard someone say “when your feet hurt, you hurt all over”? while everyone needs to give their feet attention, this is especially true for those with diabetes or blood flow problems. Nerve damage, or neuropathy, is common among people with diabetes and can cause loss of feeling in the feet. if one doesn’t feel pain, a simple injury such as a blister can become a serious infection before you find out that you have a problem. People with diabetes can also have blood flow problems, or peripheral arterial disease (Pad), which can cause injuries to heal more slowly. The good news is that there are things you can do to care for your feet. it all comes down to protecting them and being aware of any problems that occur before they become more serious. Keep your feet dry. It’s dark and moist inside your shoe, which makes it easy for bacteria to cause an infection. 7 Easy Foot Care Tips 1. Check your feet every day. Look for cuts, sores, blisters, foreign bodies (like splinters), redness or swelling around your feet and ankles and between your toes. If there is anything that is painful or looks different, call your healthcare provider immediately. 2. Keep your feet clean and moisturized. While showering, be careful not to excessively soak your feet; this can strip away the protective oils and cause them to become dry and cracked. Dry between the toes to help prevent infections, such as athlete’s foot. Use lotion to keep your feet soft and prevent against cracks or fissures. Never use lotion between the toes as it increases your risk for infection. 3. Treat cuts and sores right away. If you have a small sore or blister, use a wound wash or an antiseptic and cover with a bandage. If your sore gets worse or does not begin to heal after one-to-two days, call your foot care specialist or your primary care provider. It’s always better to be seen for a false alarm than to end up in the hospital. 4. Keep your toenails trimmed. Cut your nails straight across. If your nails are too thick or are hard to cut, a podiatrist (foot care specialist) can cut your nails and care for any thick or discolored nail tissue. If your toenails become red and infected, call your podiatrist or healthcare provider. 5. “Bathroom surgery” is never a good idea. Do not trim, shave or use over-the-counter medications to dissolve corns and calluses. The risk of doing more harm than good is just not worth it. Your podiatrist or healthcare provider can help you safely care for corns and calluses. 6. Buy shoes that fit. Shop for shoes later in the day because swelling can affect shoe fit. Ill-fitting shoes or boots can cause blisters and sores that can easily become infected. Have your feet measured from time to time to be sure your size has stayed the same. 7. Protect your feet from both hot and cold. If your feet become numb from nerve damage, you can burn your skin without knowing it. Check your bath water with your elbow rather than your toes. Be careful of hot pavements, sidewalks or sand at the beach which can also burn your feet. Avoid putting your feet on radiators, space heaters or heating pads. To protect from the cold, wear wool socks, and if your feet get wet, change your shoes and socks as soon as you can. By Guy Pupp, DPm, FACFAS ?chairman of the board?save a leg, save a life foundation
The post Some Good News For Your Feet appeared first on Spring 2016 Issue | CDiabetes Online Magazine.
]]>
The post Some Good News For Your Feet appeared first on Spring 2016 Issue | CDiabetes Online Magazine.
]]>
There is?no difference?between a pen?and a syringe?in?terms of?blood glucose?response.?It’s a?personal choice. While it’s common to?dread the thought of?taking insulin, it’s also?common to wonder why?you resisted once you get?started. If you feel ?down 33% the estimated percentage of people with?type 2 diabetes who take insulin, either alone?or in combination with diabetes pills. about taking insulin, it may?help to remind yourself?that taking insulin is not a?sign that you failed to take?care of yourself or that your?diabetes has gotten worse. It just means that your body needs insulin to keep your blood glucose levels in your target range. Pens vs. syringes Insulin can be given using either an insulin pen or a syringe. There are pluses and minuses for each. For many people, the biggest factor to consider is insurance coverage. Some insurers will not cover pens because of the cost. However, morecompanies cover pens now, so check with your insurance plan to find out if yours covers them. If you often take insulin while you’re away from home, it may be easier to carry a pen rather than a vial of insulin and a syringe. On the other hand, if you take large doses of insulin it may be easier to use a syringe. Some people feel more secure when they use a syringe because they can see the insulin leaving the syringe. Needles and syringes The good news is that needles are now smaller and thinner than ever for both pens and syringes. This means injections are less painful. Needles that are between 4-6 mm (less than ?-inch long) may be used by any adult, regardless of body weight. Be sure to give an air shot each time you use a new pen needle to make sure you get your complete dose. There is no difference in syringes in terms of accuracy or comfort. Choose the syringe size that best matches your dose and is easiest for you to read. If you take doses that end in odd numbers, choose a syringe with 1-unit markings. Giving your injection You don’t need to clean the top of the vial or your skin with alcohol. Insulin is considered bacteriostatic, which means it’s very unlikely it will give you an infection. Choose an injection site on your thighs, arms, buttocks or abdomen. Insulin is absorbed fastest from your abdomen. Your blood glucose will be more stable if you stick with one area for each type of insulin. You do need to change your injection sites slightly each day to avoid getting lumps and bumps, which interfere with insulin absorption. You don’t need to pinch an inch of skin. You can simply stick the needle straight in. With today’s shorter needles, there is almost no chance you will inject your insulin into a vein or muscle. The exceptions are children and very thin adults, who need to insert the needle at a 45-degree angle. Hold the needle in place for a count of 10 before pulling the needle out to be sure you are getting your full insulin dose. Taking it with you Unopened vials or pens can be kept in the refrigerator until the expiration date. Opened vials or the pen you are currently using don’t need to be refrigerated as long as they are at room temperature, or between 32o and 86oF. If your insulin freezes, throw it out because it will not work at all. Insulin that has been overheated will be less effective. The time this is most likely to happen is when insulin is left in a car on a cold or hot day, on a window sill or in a steamy bathroom. You can buy an insulated container to keep your insulin at the right temperature away from home. It is a good idea to think about when this is likely to happen so you can try to prevent it. It is very important to have effective insulin around when you need it. It may sound like a chore, but in the long run, it will make your life easier. ? ? 4 insulin facts ? Most people find that insulin shots are not as painful as they feared. ? If you find it painful or you often get bruises, ask your healthcare provider or educator to watch you inject yourself so he or she can offer advice. ? Some people find that pressing firmly on the injection site for a few seconds helps to ease the pain. ? Don’t worry if you see a drop of blood when you remove the needle. This does not mean that you have injected your insulin into a muscle or vein. Study Findings and what the Experts Say People who use pens are more likely to give the correct?dose and are more satisfied with taking insulin. Needles are designed to be used once, and they?get dull with each use. If you decide to reuse the?needle on your pen, change it at least once a day. Make a plan for how to take your pre-meal?insulin when away from home. By Martha Funnell, MS, RN, CDE
The post Tips For Giving Your Insulin Shot appeared first on Spring 2016 Issue | CDiabetes Online Magazine.
]]>
The post Tips For Giving Your Insulin Shot appeared first on Spring 2016 Issue | CDiabetes Online Magazine.
]]>
The intention to do something has long been thought of as a good way to measure what people actually do. In other words, people who say they are going to do something are more likely to do it. But many studies examining the intent to exercise showed a 48 percent gap between people’s intentions and their actual activity. Why Exercise Is So Hard To Do Most people have heard all about the benefits of exercise. Regular physical activity helps you look better, feel better and live longer. And if you have diabetes, you know there is an added benefit of lowering your blood glucose levels. But, for most of us, even though we want to exercise and be healthy, it still remains a struggle to get up and do it. Activity monitors are new devices that help you achieve?your fitness goals by tracking your calories, steps and?distance. Some have apps for your smart phone that can?help you track your results and keep you motivated. Making It Work For You The most important tip is to take the time to figure out what will work best for you. You are the one who knows best what will motivate you to get started with an exercise plan that you can stick to. For some people, it is exercising with a friend, and for others it is time alone. Some people do better with a class, while others prefer to exercise when they want to or in the privacy of their own homes. Some exercise early in the morning, while others prefer later in the evening to ease the stress of the day. A good way to figure out what will work for you is to come up with a list of ideas and try them out. Write down whether or not you exercised and also make note of: your blood glucose levels before and after exercise how you felt what helped you to do your exercise what got in your way 3 TIPS FOR OVERCOMING BARRIERS TO EXERCISE ? MAKE A PLANWrite it on your calendar or enter it into your smartphone. Think of exercise as an appointment you are going to keep, just as you do the other things on your schedule. ? MAKE IT A HABITHabits are things you do regularly without thinking, like brushing your teeth. You probably don’t have to think about whether you will brush your teeth before you leave the house: you just do it. When you make exercise a habit, you are less likely to talk yourself out of it—you’ll just do it. ? MAKE A BACKUP PLANNo matter how good your plan, things happen that get in the way of exercise. After all, diabetes is only one of many things on your to-do list. But if you find you’re often unable to exercise because of your schedule or other events, it’s likely that your plan is just not working. That does not mean you have failed, it just means you need to come up with a Plan B for when things get in your way. By Martha Funnell, MS, RN, CDE
The post Good Intentions appeared first on Spring 2016 Issue | CDiabetes Online Magazine.
]]>
The post Good Intentions appeared first on Spring 2016 Issue | CDiabetes Online Magazine.
]]>
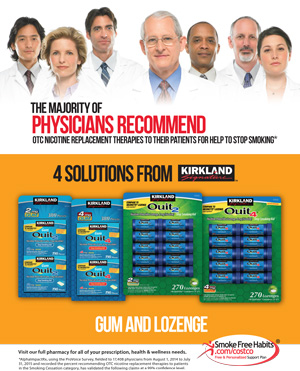
Robbie Almeida, a Costco pharmacist in Ann Arbor, Michigan, finally?quit smoking?after 15 years of advising her customers to do the same. This is how she did it. As a pharmacist, Robbie knew about the health benefits of vitamins and other supplements. She also knew that certain vitamins and supplements would help her?quit smoking. “I take a multivitamin. I take triglycerides. I take flaxseed oil, probiotics and CoQ10. And I take a calcium pill.” Robbie tells her customers at Costco pharmacy that wanting to?quit?is the first big step. For Robbie, once she made that decision, the rest followed easily. “Honestly, I just did it cold turkey. I remember I had my last cigarette at my friend’s house, and I was done. I stayed away from smoking areas so I wasn’t tempted or craving or anything like that. I wanted to?quit, so that’s how I did it. Now if I smell cigarette smoke it makes me ill. I don’t like it at all, and I think, ‘Oh, that was really gross.’ How could I have been doing that for so long?” Most people won’t be able to?quit?cold turkey like Robbie, but making that decision is an important first step. Even when she was smoking, Robbie knew that she was harming her health. Like so many people, she started smoking as a teenager. She thought “everyone” was doing it, and it seemed so cool. Then, as a pharmacist, she had to talk to her customers about the risks of smoking and advise them to?quit. It was hard to hear that smoking raises your risk of heart disease and diabetes almost every day. “The health benefits of it all–how does it make sense to put something foreign into our systems? My kids are nine and eight. They don’t remember when I was still a smoker; it’s been over 10 years. But I tell them about it so that they won’t start like I did. I tell them that it doesn’t make any sense. You’re putting something in your body that doesn’t belong there. “There’s disease. There’s pre-mature death. And the sooner you?quit, the sooner your lungs can start to recover. Back when I was smoking, I had pleurisy in my lungs, like there was an infection in the lining. Right now I feel that my lungs are probably close to 100% healthy.” Robbie?quit?soon after finishing pharmacy school. She admits that she smoked through school because of the stress. But learning about lung cancer, heart disease, strokes–she realized that it was time. She also saw what it was doing to her patients. “We measure patients’ lung capacity, and every year or so and I have to talk to the smokers about the benefits of?stopping.?You can tell right away when they blow into the tube and they can’t breathe that they have had decades of smoking. It’s really bad. And then of course they have to rely on drugs, like inhalers, and everything else that goes along with smoking-related diseases, and all that is very costly. So, it doesn’t make any sense. “I’ve had patients come to me with nicotine gum and ask me whether it works or not. I tell them that they have to be willing to quit, because if they’re not, nothing will really work. I haven’t been monitoring exactly how many patches or over-the-counter products people are buying now thanks to their New Year’s resolutions, but more people are coming to the pharmacy and talking to me about?quitting. “I believe in determination. In my mind I was done smoking, so that’s why I was able to?quit. It’s up to each individual to realize the benefits of?quitting?and to decide how to do it. A lot of people use the gum or the patch. That’s fine. With the gum, heavy smokers can start off with a higher dosage to decrease the craving, and then gradually decrease the dose as they start smoking less. They taper down until they get to the lower dose and then, hopefully, the cravings won’t be there and they will have?quit.” Family history also plays a role. Robbie’s father smoked until she was born. Like Robbie, he?stopped?before his children saw him smoking. But Robbie’s grandfather smoked and great grandmother also smoked. Robbie’s grandfather died of complications from smoking; most likely, it aggravated his heart disease. Robbie has been taking calcium ever since she finished school to avoid osteoporosis. She wants to keep strong bones so that she’ll be healthy for his children “A lot of older smokers don’t think like that. They are pretty much addicted and they can’t stop. My children are always on my mind. I have to be healthy for them, so everything that I’m doing is so that I can be with them longer.” By?Jonathan Jarashow
The post Quitting Smoking: A Costco pharmacist’s story appeared first on Spring 2016 Issue | CDiabetes Online Magazine.
]]>
 Robbie Almeida, a Costco pharmacist in Ann Arbor, Michigan, finally?quit smoking?after 15 years of advising her customers to do the same. This is how she did it.
Robbie Almeida, a Costco pharmacist in Ann Arbor, Michigan, finally?quit smoking?after 15 years of advising her customers to do the same. This is how she did it.
As a pharmacist, Robbie knew about the health benefits of vitamins and other supplements. She also knew that certain vitamins and supplements would help her?quit smoking.
“I take a multivitamin. I take triglycerides. I take flaxseed oil, probiotics and CoQ10. And I take a calcium pill.”
Robbie tells her customers at Costco pharmacy that wanting to?quit?is the first big step. For Robbie, once she made that decision, the rest followed easily.
“Honestly, I just did it cold turkey. I remember I had my last cigarette at my friend’s house, and I was done. I stayed away from smoking areas so I wasn’t tempted or craving or anything like that. I wanted to?quit, so that’s how I did it. Now if I smell cigarette smoke it makes me ill. I don’t like it at all, and I think, ‘Oh, that was really gross.’ How could I have been doing that for so long?”
Most people won’t be able to?quit?cold turkey like Robbie, but making that decision is an important first step.
Even when she was smoking, Robbie knew that she was harming her health. Like so many people, she started smoking as a teenager. She thought “everyone” was doing it, and it seemed so cool. Then, as a pharmacist, she had to talk to her customers about the risks of smoking and advise them to?quit. It was hard to hear that smoking raises your risk of heart disease and diabetes almost every day.
“The health benefits of it all–how does it make sense to put something foreign into our systems? My kids are nine and eight. They don’t remember when I was still a smoker; it’s been over 10 years. But I tell them about it so that they won’t start like I did. I tell them that it doesn’t make any sense. You’re putting something in your body that doesn’t belong there.
“There’s disease. There’s pre-mature death. And the sooner you?quit, the sooner your lungs can start to recover. Back when I was smoking, I had pleurisy in my lungs, like there was an infection in the lining. Right now I feel that my lungs are probably close to 100% healthy.”
Robbie?quit?soon after finishing pharmacy school. She admits that she smoked through school because of the stress. But learning about lung cancer, heart disease, strokes–she realized that it was time. She also saw what it was doing to her patients.
“We measure patients’ lung capacity, and every year or so and I have to talk to the smokers about the benefits of?stopping.?You can tell right away when they blow into the tube and they can’t breathe that they have had decades of smoking. It’s really bad. And then of course they have to rely on drugs, like inhalers, and everything else that goes along with smoking-related diseases, and all that is very costly. So, it doesn’t make any sense.
“I’ve had patients come to me with nicotine gum and ask me whether it works or not. I tell them that they have to be willing to quit, because if they’re not, nothing will really work. I haven’t been monitoring exactly how many patches or over-the-counter products people are buying now thanks to their New Year’s resolutions, but more people are coming to the pharmacy and talking to me about?quitting.
“I believe in determination. In my mind I was done smoking, so that’s why I was able to?quit. It’s up to each individual to realize the benefits of?quitting?and to decide how to do it. A lot of people use the gum or the patch. That’s fine. With the gum, heavy smokers can start off with a higher dosage to decrease the craving, and then gradually decrease the dose as they start smoking less. They taper down until they get to the lower dose and then, hopefully, the cravings won’t be there and they will have?quit.”
Family history also plays a role. Robbie’s father smoked until she was born. Like Robbie, he?stopped?before his children saw him smoking. But Robbie’s grandfather smoked and great grandmother also smoked. Robbie’s grandfather died of complications from smoking; most likely, it aggravated his heart disease. Robbie has been taking calcium ever since she finished school to avoid osteoporosis. She wants to keep strong bones so that she’ll be healthy for his children
“A lot of older smokers don’t think like that. They are pretty much addicted and they can’t stop. My children are always on my mind. I have to be healthy for them, so everything that I’m doing is so that I can be with them longer.”
By?Jonathan Jarashow
The post Quitting Smoking: A Costco pharmacist’s story appeared first on Spring 2016 Issue | CDiabetes Online Magazine.
]]>
Pepare, portion and pack your own lunch so you can enjoy a healthy midday meal at work or school. Do you often feel pressured to order the same type of food as your friends or co-workers? Try to make your own food choices. If you pack your own lunch, then you can decide what’s on your midday menu.?If you buy lunch, you might be restricted to local restaurants with limited menus or vending machines. Think about how much money you could save if you bring your lunch. You’ll also be in control of your carbohydrate and calorie budget. In addition, packing a healthy lunch can help you lose weight, reduce midday fatigue and control your blood glucose levels. 10 TIPS FOR PACKING YOUR LUNCH 1 Use a padded (insulated) bag.Put a frozen ice pack on the bottom. A reusable padded bag will help keep your food at the right temperature. 2 Plan your lunch menus.Write down your shopping list before you go to the market. When you plan your menus, don’t forget to include lean protein (such as chicken, turkey or fish) and plenty of vegetables. Choose colorful, low-calorie vegetables, which have plenty of fiber. This will help fill you up so you won’t eat too many calories. 3 Be creative.Don’t settle for a dry turkey sandwich on boring, low-fiber white bread. Bring a thermos of hearty vegetable soup with turkey meatballs for lunch on a cold winter day. You can cook the soup over the weekend and freeze it in portions. Or try some crunchy whole grain crackers with last night’s leftover salmon and sliced cucumber. 4 Prepare your lunch the night before. Store your padded bag near the fridge. That way you’ll never forget to bring your lunch, and you will save time in the morning. 5 Bring a plastic or metal water bottle to work or school. Refill your bottle every few hours. Then take it home to reuse again. For extra flavor, add a sugar-free, calorie-free powder mix, or squeeze a little lemon or lime into your water. You’ll quench your thirst without adding calories or carbohydrates. 6 Use your leftovers. Prepare a little extra for dinner, and bring the leftovers for lunch. Here’s one idea: cook an extra portion of grilled chicken with quinoa over steamed broccoli and bring it for lunch. 7 Measure your food in advance. This helps save time and may help you control your weight and blood glucose levels. Keep an honest food journal. Write down what you spend on food purchases. Soon you’ll see how much money you save when you bring your own healthy lunch from home. 8 Bring your salad or left overs in a bag or reusable container.You’ll save money and help protect the environment at the same time. 9 Savor your salads.Prepare enough salad for two days. Use lots of veggies. Here’s a great salad idea: Mix romaine lettuce, cucumbers, radishes, mushrooms, red cabbage and a few grape tomatoes. Add some diced grilled chicken or turkey breast and toss in some chick peas. Top your salad off with a few chopped walnuts. Pack a small side of olive oil and vinegar to add when you’re ready for lunch. Finish off your meal with some fresh berries or a crisp apple. 10 Pat yourself on the back.When you pack your lunch, you make it easier for yourself to avoid unhealthy fast food choices, such as hamburgers and fries or fried chicken and creamy mashed potatoes that are loaded with carbohydrates, unhealthy fat, sodium and calories. ? By Susan Weiner, MS, RDN, CDE, CDN
The post Pack A Healthy Lunch appeared first on Spring 2016 Issue | CDiabetes Online Magazine.
]]>
The post Pack A Healthy Lunch appeared first on Spring 2016 Issue | CDiabetes Online Magazine.
]]>